What Is Plantar Fasciitis?

Plantar fasciitis is a common cause of heel pain, occurring when the thick band of tissue that runs along the bottom of the foot becomes inflamed. It is often caused by repetitive strain, such as from excessive walking, running, or wearing poorly fitting shoes. Other contributing factors include obesity, tight calf muscles, or an abnormal foot arch. The primary symptom of plantar fasciitis is sharp heel pain, particularly when taking the first steps in the morning or after long periods of sitting. The pain may subside with activity but often returns after prolonged standing or exercise. Treatment for plantar fasciitis focuses on reducing inflammation and relieving pressure. Common methods include stretching exercises, anti-inflammatory medications, and custom orthotics. In severe cases, corticosteroid injections may be recommended. A podiatrist can provide a comprehensive treatment plan tailored to your needs, helping you recover and prevent future flare-ups. If you are experiencing persistent heel pain, it is suggested that you schedule an appointment with a podiatrist for expert care.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Premier Ankle & Foot Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in South York, West York, and East York, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
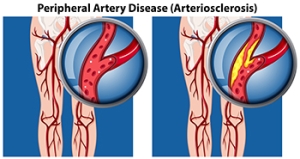
Foot Symptoms and Complications of PAD
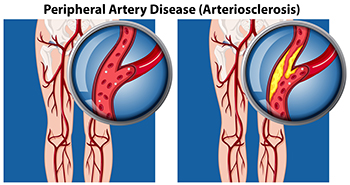
Peripheral artery disease, or PAD, is a serious condition where narrowed arteries limit blood flow to the limbs, and especially affects the feet. People with peripheral artery disease may experience a persistent cold sensation in their feet, even in warm environments, due to restricted blood circulation. Tingling, numbness, or loss of sensation, especially in the toes, can signal nerve strain caused by reduced oxygen supply. Additionally, skin on the feet may turn pale or develop a bluish tint as circulation diminishes. Peripheral artery disease can also slow toenail growth, leading to thicker, brittle nails that may appear discolored. In advanced cases, patients with PAD might develop painful sores or ulcers on the feet that are slow to heal, increasing the risk of infection and severe complications. A podiatrist can identify signs of peripheral artery disease and help patients manage foot health. If you have foot pain that derives from circulatory issues, it is suggested that you make an appointment with a podiatrist for appropriate treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Premier Ankle & Foot Specialists. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in South York, West York, and East York, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Top 5 Benefits of Custom Orthotics

Discover the long-term benefits of orthotics! Tailored to your unique foot structure, Custom Orthotics ensure every step radiates comfort and helps reduce foot and heel pain. Beyond comfort, they enhance your posture, allowing you to stand taller and walk with confidence. Whether you're casually strolling or actively running, they can elevate your performance. Call our office today and see if Custom Orthotics are right for you.
All About Corns on the Feet

Corns are dense patches of hardened skin that develop on the feet, often as a response to pressure and friction. Corns commonly form on the top or sides of toes or the outer edge of the foot, typically where footwear consistently rubs. High heels, wearing tight or poorly fitted shoes, and even walking without socks can contribute to corn formation by creating repeated friction. Corns are distinct from calluses due to their smaller, deeper size and hard core surrounded by inflamed skin, which can be painful when pressure is applied. Symptoms of corns include a rough, raised bump, tender skin, and occasional flakiness. A podiatrist can diagnose a corn through visual examination, ensuring that other conditions like cysts or warts are ruled out. Professional treatment includes carefully trimming the thickened skin, applying medicated patches, and possibly prescribing custom orthotics to prevent recurrence. If you have developed a painful corn, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
If you have any concerns regarding your feet and ankles, contact one of our podiatrists of Premier Ankle & Foot Specialists. Our doctors will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctors to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in South York, West York, and East York, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns: What Are They, and How Do You Get Rid of Them
Corns are thickened areas on the skin’s surface, to the point of being irritating and sometimes painful. Commonly found on the feet, corns are circular or cone-shaped. They develop where there are areas of pressure or friction, such as on the little toe when it rubs up against shoes, or on the ball of your foot.
Corns are often confused with a callus, but there is a difference between them. Corns can be raised bumps that are painful to the touch. They consist of a rough, thick area of skin that may be dry or waxy. Corns tend to be surrounded by skin that is inflamed, and are usually much smaller than calluses.
Removing the dead skin that has built up is the key in treating corns. Salicylic acid medication is most common in accomplishing this. The acid works by dissolving keratin, which is the protein that makes up the majority of corns. You can purchase salicylic acid over-the-counter in products such as wart removers. It comes in a variety of forms such as medicated pads, drops, or creams. However, people who are diabetic should not use salicylic acid, but should instead consult their doctor immediately.
According to the product directions, applying the medication directly onto the corn will treat it. The top layer of the corn will begin to turn white after use. When that occurs, the layers of skin can then be peeled away, making the corn smaller. Shaving off corns with razors or other pedicure equipment is never a good idea. This can lead to infection. If your corn gets infected, and is not treated immediately, a visit to the doctor will be necessary.
Another way to treat corns and help prevent their return is by using orthotic inserts, fitted by a podiatrist. Inserts fit right into your shoes and adjusts the way your foot fits into your shoes. This fixes the way you walk. This will lower your chances of getting corns, and eliminate current corns by reducing rubbing from friction.
Surgery is rarely used to treat corns, but does occur on occasion. Surgery actually deals with the underlying issue that causes corns. During surgery, the bone is shaved and any abnormalities are corrected, thus reducing the amount of friction that occurs during walking.
To prevent corns, the first step is reducing friction. Always wear shoes that fit well and don’t rub your feet. Pads can be purchased if you notice rubbing developing. These pads can be purchased over-the-counter, and can be simply placed on the irritated area. Wearing cushioned insoles in your shoes can always reduce the friction, and making sure to wear well-fitting shoes. This will ensure that your foot is not being squeezed awkwardly, and prevent corns from forming in the first place.
Benefits of Custom Orthotics for Flat Feet

Custom orthotics are often recommended for people with flat feet, offering a more tailored solution compared to off-the-shelf options. While over-the-counter orthotics may provide relief for some, they come in a limited range of sizes and lack the personalized fit needed for many flat-footed individuals. This can lead to inadequate support and discomfort over time. In contrast, custom-made orthotics are specifically designed for each person's unique foot shape, providing better support and alignment. This makes them ideal for both typical and atypical cases of flat feet. The process of creating custom orthotics takes time, requiring multiple adjustments and a longer manufacturing period to ensure the best fit, but the process is becoming shorter with technological advancements. If you have uncomfortable flat feet, it is suggested that you schedule an appointment with a podiatrist to see if custom orthotics can help you.
The benefits of custom orthotics are far-reaching and can make a significant impact on your daily life. Whether you are an athlete looking to enhance your performance, a healthcare worker on your feet every day, someone who experiences chronic foot pain, or someone who wants to improve their overall comfort and well-being, custom orthotics can be a game changer.
Custom orthotics provide support, stability, and relief for a variety of foot conditions ranging from flat feet to heel pain. They can even help prevent injuries and address more severe foot concerns, such as plantar fasciitis and diabetic foot issues.
Contact one of our podiatrists at Premier Ankle & Foot Specialists to create tailored orthotics for you and enjoy a higher quality of life, reduced pain, and increased mobility. With the right orthotics, you can continue doing the things you love, whether it’s running, dancing, or simply walking comfortably without discomfort.
If you are suffering from foot discomfort or have concerns about your foot health, do not hesitate to contact one of our podiatrists at Premier Ankle & Foot Specialists to explore the benefits of orthotics for you. Your feet are the foundation of your body and investing in their well-being can lead to a happier, healthier, and more active lifestyle. Your feet will thank you!
If you have any questions please contact our offices located in South York, West York, and East York, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Wearing the Right Shoes on Construction Sites

Wearing the right shoes on construction sites is essential for ensuring safety and comfort. Proper footwear is designed to provide adequate support, protection, and traction on uneven surfaces. Construction environments often expose workers to heavy machinery, sharp objects, and potential slip hazards, making sturdy shoes vital for preventing injuries. Steel-toed boots, for example, protect against falling objects, while slip-resistant soles reduce the risk of slips and falls. Additionally, appropriate footwear can help alleviate fatigue during long hours on the job, while promoting better posture and reducing strain on the feet and legs. Investing in high-quality work shoes not only enhances safety but also improves overall job performance. If you have endured a foot injury while at work, it is suggested that you contact a podiatrist who can offer you a diagnosis and treatment solutions, in addition to discussing correct footwear choices.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact one of our podiatrists from Premier Ankle & Foot Specialists. Our doctors will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our offices located in South York, West York, and East York, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.